In parts one and two of our series on breast/chest feeding problems, our midwife Katrin Ritter explained what makes a good start to breast/chest feeding and how correct latching on works.
But what happens if you still can't cope or you have one or two other problems? In hospitals there are often trained breastfeeding counsellors (IBCLC) who have thorough training and can help. Otherwise, a midwife with breast/chest feeding experience, or breast/chest feeding support networks can always help.
Here are some of the most common reasons for early weaning.
What can have a negative effect on breast/chest feeding:
- Oxytocin administration during birth as a medicine. This can disrupt the maternal oxytocin system, but also have an influence on the baby's reflexes and immune system.
- Painkillers (opioids) and anaesthesia for the mother.
- A surgical delivery by caesarean section. You will need rest with limited movement to allow recovery.
- Artificial teats, nipples and soothers. If possible, avoid them completely for the first 4 to 6 weeks to prevent feeding confusion.

Some women stop breast/chest feeding because they feel pain. But is that actually normal? And how much do we have to put up with?
In the first few days, you will experience pain while breast/chest feeding. This can last for a few days and is intensified as oxytocin, which promotes labour, is released during breast/chest feeding. Your nipples may be sensitive and slightly sore during this period too.
During the first one to three weeks, you may feel pain at the beginning of your breast/chest feeding session. This may last up to 30 seconds per session until your milk-supply reflex sets in. This is caused by the pulling sensation in your nipples and breasts/chest and is considered normal. After that, the pain should stop.
However, there are some reasons why breast/chest feeding may cause you persistent pain or not work properly. In these cases, it is important to talk to your midwife or breast/chest feeding consultant.
The most common breast/chest feeding problems in early labour.
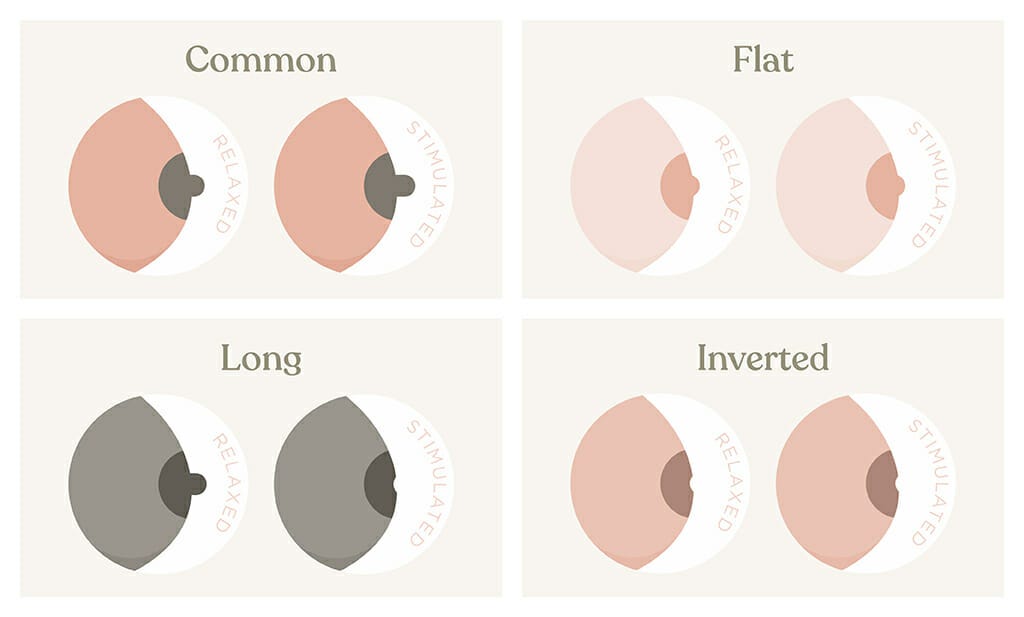
There are three different shapes of nipples. Flat, inverted, and long nipples.
It is important that you latch on correctly with your unquie nipple shape. Your baby doesn't know any other nipple shape and in most cases will have no problem.
For example, before breast/chest feeding, you can pump briefly to make your nipple stand out a bit more. Tools like nipple shapers can also help. Please keep your nipple clean and dry and do not use nipple shields. If you need to feed, only use a spoon or cup.
Unfavourable weight development in your child.
Your child should not lose more than 7% body weight in the first few days after birth. In the case of exclusively breast/chest fed children, the low point is usually reached on the third day.
However, birth weight should be reached again by the 10th day, or the very latest, 14th day. As a guideline, your child will then gain about 30 grams of weight per day.
What can you do to promote this?
Skin contact, breast/chest feeding as needed, and at least every two hours - four hours off at night is okay. It is important to offer both breasts/chest in different breast/chest feeding positions for each feed. Please do not to use artificial teats, or give your little one formula at first in case of breast/chest milk shortage. You can contact your midwife, lactation consultant or paediatrician and ask for help.
Excessive onset of copious milk production.
This causes sore and tense breasts/chest which is caused by increased blood flow, onset of copious milk production and lymph congestion. Frequent and correct breast/chest feeding is preventive.
What can you do?
After breast/chest feeding, use a cooling compresses for at least 20 minutes. For example, frozen peas/corn, cool pack stored in the fridge, not the freezer.
Top Tip : Place a cloth between the pad and your breast/chest . You can also perform a breast/chest massage according to the breast/chest feeding counsellor's instructions.
Newborn jaundice. A rise in jaundice levels up to a certain limit is normal in the first 5-7 days. If it is too high, it will be checked by the midwife or paediatrician and your baby may need to be treated with light therapy. Breast/chest feeding as needed and early first lactation have a preventive effect.
Insufficient milk production. Lack of milk is the reason for premature weaning for one third of women. However, over 95% of women are physically able to breast/chest feed their child sufficiently. Therefore consult a lactation consultant IBCLC or midwife and do not give up immediately.
Excessive supply of breast milk. This can lead to swallowing, changes in sucking behaviour, repeatedly letting go of the breast/chest, crying and rejection. Further consequences can be milk congestion, breast/chest infections and early weaning.
Often the amount regulates itself after a few weeks. In any case, a specialist should be consulted. Sage tea and cooling the breast/chest after breast/chest feeding can also have a milk-inhibiting effect.

Milk engorgement and breast/chest inflammation. Here there is pain, hardening, redness, fever and discomfort. Contact your midwife or breast/chest feeding counsellor. In case of milk engorgement, please seek medical treatment after 24 hours if the symptoms worsen.
All of the above reasons can lead you to give up breast/chest feeding prematurely. Even though it not only offers your child the best nutrition, but also strengthens your bond and has a positive influence on their development.
Therefore seek advice from a professional early on. Breast/chest feeding should neither hurt nor be a struggle. An experienced lactation consultant can most likely help you save your breast/chest feeding relationship.